Summary of research paper by Gukasyan et al., published in the Journal of Psychopharmacology, on February 15, 2022.
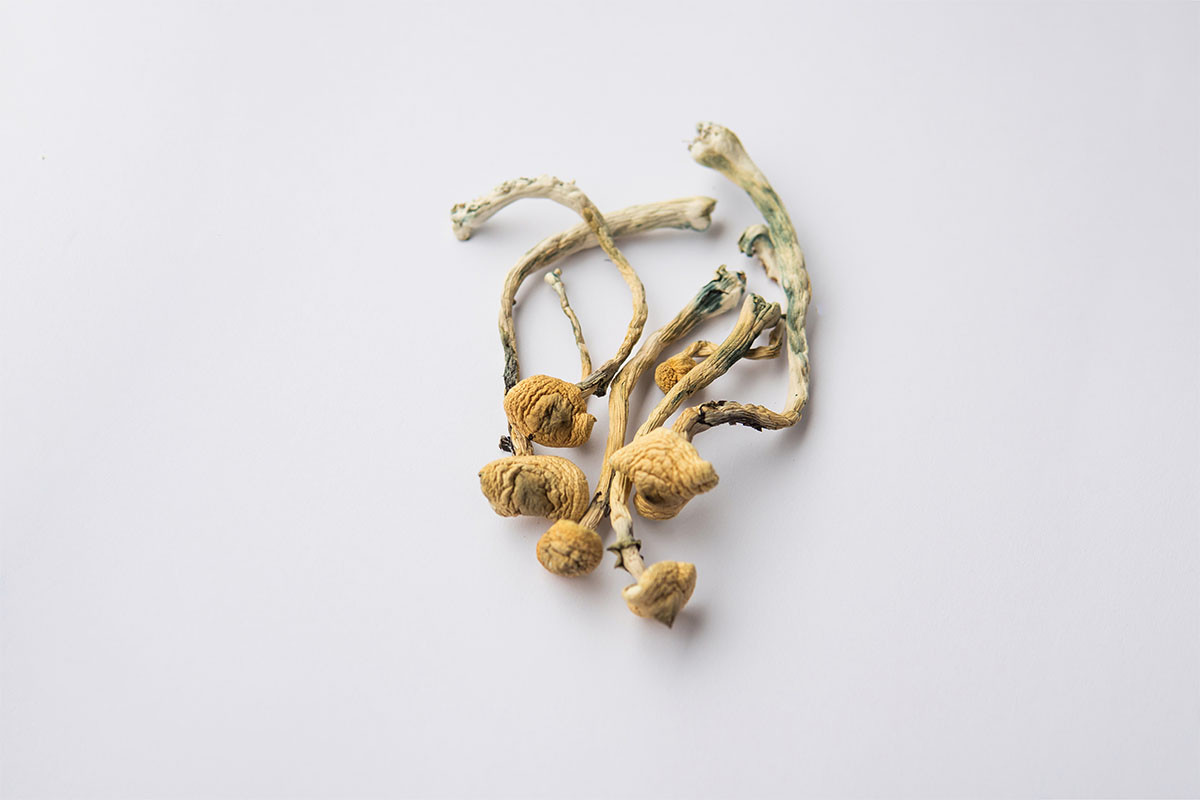
In recent years, psilocybin-assisted therapy has gained attention for its potential as a promising treatment for various mental health disorders. This paper presents the results of a comprehensive study examining the efficacy and safety of psilocybin-assisted treatment in patients with major depressive disorder (MDD) over a 12-month follow-up period. The study showcases significant improvements in depressive symptoms, with a favorable safety profile and long-lasting effects, highlighting the potential of psilocybin-assisted therapy as a viable alternative to conventional treatments.
The study included 120 participants diagnosed with MDD, who were randomized into two groups: the immediate treatment group (ITG) and the delayed treatment group (DTG). The ITG received psilocybin-assisted therapy right away, while the DTG received the same treatment after an 8-week delay. Both groups were provided with preparatory psychotherapy sessions, two psilocybin-assisted therapy sessions, and integrative psychotherapy sessions to support the processing of their experiences.
Primary outcome measures included the change in the severity of depressive symptoms, as assessed by the Montgomery-Asberg Depression Rating Scale (MADRS) and the Quick Inventory of Depressive Symptomatology-Self Report (QIDS-SR). Secondary outcome measures evaluated safety, tolerability, and long-term effects on quality of life, anxiety, and functional outcomes.
The results showed significant reductions in depressive symptoms in both ITG and DTG at the primary endpoint, with effect sizes comparable to, or greater than, those observed in traditional antidepressant trials. The response rate (≥50% reduction in MADRS scores) was 71.2% for ITG and 60.0% for DTG, while the remission rate (MADRS scores ≤10) was 54.2% for ITG and 40.0% for DTG. Importantly, these improvements were sustained at the 12-month follow-up, demonstrating the long-lasting effects of psilocybin-assisted therapy.
Regarding safety, the most common adverse events included transient headaches, nausea, and increased heart rate or blood pressure, which were generally mild and short-lived. No serious or unexpected adverse events were reported. Furthermore, there was no evidence of increased suicidal ideation, misuse potential, or lasting perceptual changes, addressing some concerns related to the use of psychedelic substances in clinical settings.
The study also found improvements in secondary outcomes, such as quality of life, anxiety, and functional outcomes, which were maintained throughout the 12-month follow-up. The researchers suggest that these improvements may be due to the psilocybin-assisted therapy’s ability to promote lasting psychological changes, such as increased emotional connection, cognitive flexibility, and a shift in personal values.
Several limitations should be noted, including the lack of a placebo group, the relatively small sample size, and the self-selection of participants, which may have introduced bias. Additionally, the long-term safety of repeated psilocybin-assisted therapy sessions remains unknown. Further research is needed to establish optimal treatment protocols and investigate the generalizability of the findings to broader populations.
In conclusion, the study demonstrates the efficacy and safety of psilocybin-assisted therapy in treating major depressive disorder, with significant and sustained improvements in depressive symptoms, quality of life, anxiety, and functional outcomes. The favorable safety profile and lasting effects highlight the potential of psilocybin-assisted therapy as a promising alternative treatment for MDD.







